PRIMARY CARE THERAPEUTICS VOL 1
| Site: | BIOSOFT EDUCATIONAL RESOURCES - Authored by Dr Ananda Perera |
| Course: | BIOSOFT HELP FILES |
| Book: | PRIMARY CARE THERAPEUTICS VOL 1 |
| Printed by: | Guest user |
| Date: | Saturday, 20 December 2025, 1:52 AM |
Description
THIS HAND BOOK GIVES ALL THE PRINCIPLES AND THE ACTIONS REQUIRED FROM GENERAL PRACTITIONERS TO INDUCE RECOVERY FROM ILLNESSES IN THEIR PATIENTS
Table of contents
- 1. INTRODUCTION
- 2. DESCRIPTION
- 3. PRINCIPLES UNDERLYING
- 4. PCT EXECUTION
- 5. MONITORING NATURAL HISTORY
- 6. CAUSES OF RECOVERY FROM ILLNESS
- 6.1. MORE CAUSES OF RECOVERY
- 6.2. PROPOSED HIERARCHY OF ACTIONS
- 6.3. DEVIATIONS FROM NATURAL REMISSION
- 6.4. FACTORS IMPACTING NATURAL HISTORY OF DISEASE
- 6.5. HOWTO INDUCT NATURAL REMISSION
- 6.6. EBM NEEDS SATISFACTION
- 6.7. LIVED EXAMPLES FROM GENERAL PRACTICE
- 6.8. DYNAMICS OF ILLNESS RECOVERY
- 6.9. ILLNESS RECOVERY IMPERATIVES
- 6.10. GUIDING PATIENT TO RECOVERY
- 6.11. DRUG PHARMACOLOGY
- 7. PLACEBO
- 7.1. DEFINTIONS AND CONSENSUS
- 7.2. OVERVIEW OF PLACEBO
- 7.3. PLACEBO GENESIS
- 7.4. CONDITIONING
- 7.5. PLACEBO AND PLACEBO EFFECTS
- 7.6. EMPATHY HOWTO
- 7.7. PLACEBO EXAMPLES
- 7.8. EXPECTANCY EFFECTS
- 7.9. INDUCTION OF EXPECTANCY
- 7.10. MEANING AS PLACEBO
- 7.11. PLACEBOGENIC PHYSICIAN
- 7.12. REWARDS AS PLACEBO
- 7.13. DEVELOP A REWARD SYSTEM
- 7.14. IMAGE OF SUCCESS - SYMBOLISM
- 8. NOCEBO EFFECTS
- 9. BIAS - PATIENT, PHYSICIAN, SOCIAL
- 9.1. INTRODUCTION
- 9.2. BIAS AND EMOTIONS
- 9.3. BIAS AND SOMATIZATION
- 9.4. BIAS AND DECISION MAKING
- 9.5. BIAS MANAGEMENT HOWTO
- 9.6. HAWTHORNE EFFECT
- 9.7. HAWTHORNE IMPLEMENTATION
- 9.8. HALO EFFECT
- 9.9. HALO EFFECT IMPLEMENTATION
- 9.10. JASTROW EFFECT
- 9.11. JASTROW IMPLEMENTATION
- 9.12. PYGMALION EFFECT
- 9.13. PYGMALION MECHANISM
- 9.14. PYGMALION IMPLEMENTATION
- 9.15. REFERENCES
- 10. REGRESSION TO MEAN
- 11. THERAPEUTIC RELATIONSHIP DYNAMICS
- 12. PATIENT PHYSICIAN RELATIONSHIP
- 12.1. PATIENT PHYSICIAN RELATIONSHIP NATURE
- 12.2. WHAT IS IT AND WHAT IT IS NOT
- 12.3. SKILLS REQUIRED FOR A GP
- 12.4. SIGNS OF HIGH SKILL LEVEL
- 12.5. HIGH SKILL LEVEL IN EMOTIONS MANAGEMENT
- 12.6. BASIC CONTENTS OF PATIENT PHYSICIAN RELATIONSHIP
- 12.7. OPTIMAL PPR DEVELOPMENT
- 12.8. OPTIMAL PPR PATIENT CENTERDNESS
- 12.9. PPR AND COMMUNICATION SKILLS
- 12.10. MIRRORING TECHNIQUES FROM NLP
- 12.11. OPTIMAL PPR DEVELOPMENT
- 12.12. PATIENT PHYSICIAN RELATIONSHIP DEVELOPMENT
- 12.13. RELATIONSHIP DEVELOPMENT CONTINUED
- 12.14. THERAPEUTIC RELATIONSHIP TYPES
- 12.15. WORKING ALLIANCE
- 12.16. TRANSFERENCE AND COUNTERTRANSFERENCE
- 12.17. REPARATIVE RELATIONSHIPS
- 12.18. PERSON TO PERSON RELATIONSHIP
- 12.19. TRANSPERSONAL RELATIONSHIPS
- 12.20. MECHANISMS OF THERAPEUTIC EFFECTS
- 12.21. PHYSICIAN EMPATHY
- 12.22. medication adherence
- 12.23. PATIENT ENGAGEMENT
- 13. SOCIAL SUPPORT IN PCT
- 14. HUMAN BEHAVIOR CHANGE INTRODUCTION
- 14.1. IMPLEMENTATION OF HEALTH BEHAVIOR CHANGES
- 14.2. THERAPEUTIC LIFESTYLE CHANGES
- 14.3. HEALTH BEHAVIOR CHANGE HOWTO
- 14.4. HEALTH BEHAVIOR MODEL
- 14.5. HEALTH BEHVAIOR MODEL THEORY
- 14.6. LIKELIHOOD OF FOLLOWING PHYSICAN ADVICE
- 14.7. PERCEIVED THREAT OF DISEASE
- 14.8. CUES TO ACTION IN HBM
- 14.9. FACTORS MODIFYING THE PERCEPTIONS
- 14.10. INCREASING THE COMPLIANCE FOR VACCINATION
- 14.11. HEALTH MOTIVATION
- 14.12. WHATIS SELF SUSCEPTIBILITY
- 14.13. PERCEPTIONS AND CUES FOR ACTION
- 14.14. EXTERNAL CUES FOR ACTION
- 14.15. CONSULTATION VARIABLES
- 14.16. MANAGEMENT OF HEALTH RELATED BEHAVIORS
- 14.17. CRITIQUE OF HBM
- 14.18. PRECEDE AND PROCEDE MODEL
- 14.19. PRECEDE
- 14.20. PRECEDE STRUCTURE
- 14.21. WHATIS PROCEDE
1. INTRODUCTION

2. DESCRIPTION
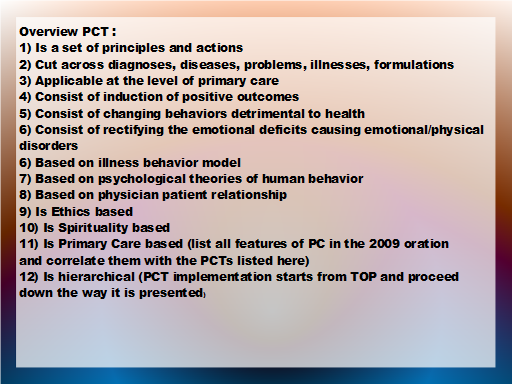
3. PRINCIPLES UNDERLYING
4. PCT EXECUTION
4.1. PCT DYNAMICS
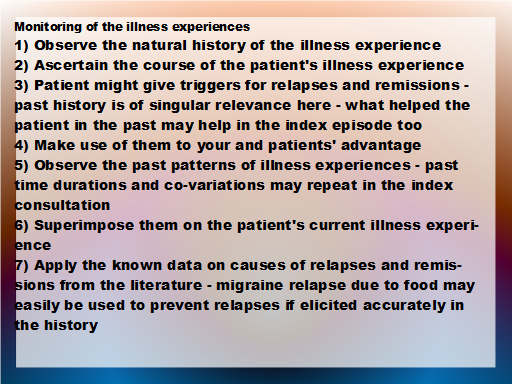
5. MONITORING NATURAL HISTORY
6. CAUSES OF RECOVERY FROM ILLNESS
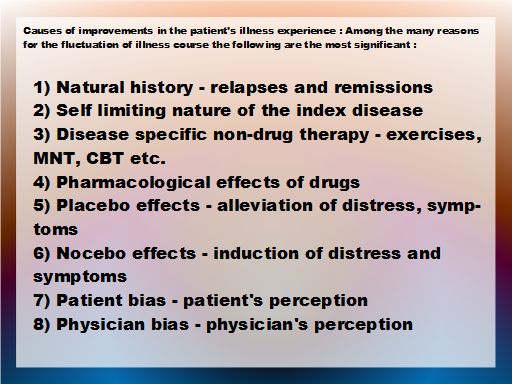
6.1. MORE CAUSES OF RECOVERY
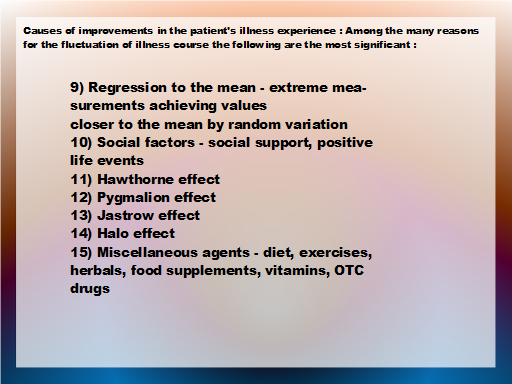
6.2. PROPOSED HIERARCHY OF ACTIONS
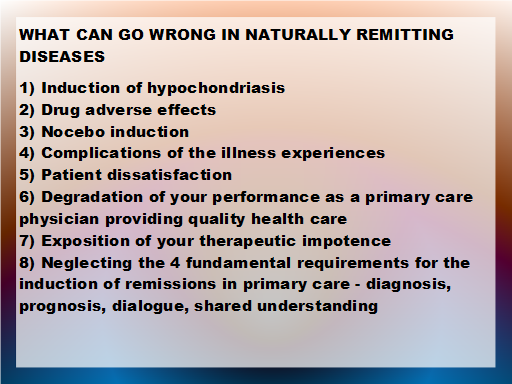
6.3. DEVIATIONS FROM NATURAL REMISSION
6.4. FACTORS IMPACTING NATURAL HISTORY OF DISEASE
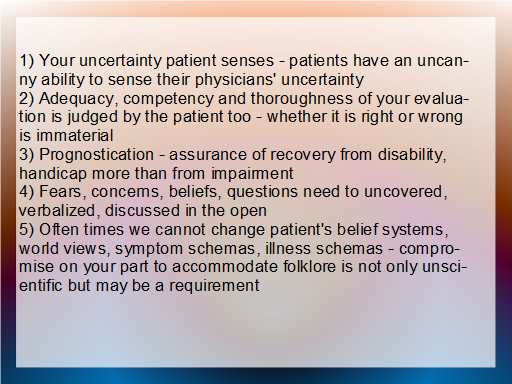
6.5. HOWTO INDUCT NATURAL REMISSION
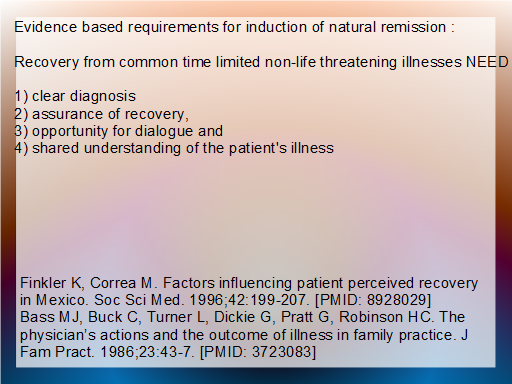
6.6. EBM NEEDS SATISFACTION
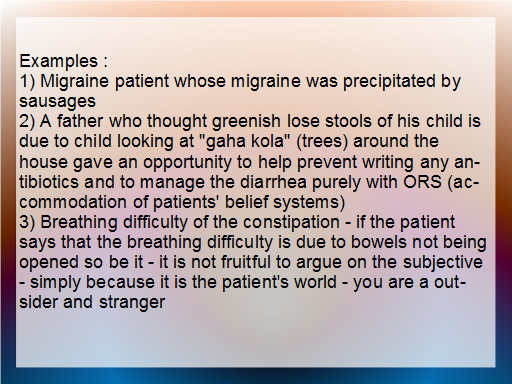
6.7. LIVED EXAMPLES FROM GENERAL PRACTICE
6.8. DYNAMICS OF ILLNESS RECOVERY
6.9. ILLNESS RECOVERY IMPERATIVES
6.10. GUIDING PATIENT TO RECOVERY
6.11. DRUG PHARMACOLOGY
7. PLACEBO
7.1. DEFINTIONS AND CONSENSUS
7.2. OVERVIEW OF PLACEBO
7.3. PLACEBO GENESIS
7.4. CONDITIONING
7.5. PLACEBO AND PLACEBO EFFECTS
7.6. EMPATHY HOWTO
7.7. PLACEBO EXAMPLES
7.8. EXPECTANCY EFFECTS
7.9. INDUCTION OF EXPECTANCY
7.10. MEANING AS PLACEBO
7.11. PLACEBOGENIC PHYSICIAN
7.12. REWARDS AS PLACEBO
7.13. DEVELOP A REWARD SYSTEM
7.14. IMAGE OF SUCCESS - SYMBOLISM
8. NOCEBO EFFECTS
8.1. WHAT IS NOCEBO
8.2. CONTEXTUAL FACTORS
8.3. NOEBO VICIOUS CIRCLE
8.4. NOCEBO CAUSATION
8.5. EXAMPLES NOCEBO
8.6. NOCEBO GENESIS
8.7. NOCEBO GENESIS CONTINUED
8.8. PREVENTION OF NOCEBO IN GP
8.9. NOCEBO MANAGEMENT
9. BIAS - PATIENT, PHYSICIAN, SOCIAL
9.1. INTRODUCTION
9.2. BIAS AND EMOTIONS
9.3. BIAS AND SOMATIZATION
9.4. BIAS AND DECISION MAKING
9.5. BIAS MANAGEMENT HOWTO
9.6. HAWTHORNE EFFECT
9.7. HAWTHORNE IMPLEMENTATION
9.8. HALO EFFECT
9.9. HALO EFFECT IMPLEMENTATION
9.10. JASTROW EFFECT
9.11. JASTROW IMPLEMENTATION
9.12. PYGMALION EFFECT
9.13. PYGMALION MECHANISM
9.14. PYGMALION IMPLEMENTATION
9.15. REFERENCES
10. REGRESSION TO MEAN
10.1. REGRESSION TO MEAN CLINICALS
10.2. CLINICALS
10.3. REGRESSION TO MEAN ALERT
10.4. OVERCOMING REGRESSION TO MEAN
11. THERAPEUTIC RELATIONSHIP DYNAMICS
12. PATIENT PHYSICIAN RELATIONSHIP
12.1. PATIENT PHYSICIAN RELATIONSHIP NATURE
12.2. WHAT IS IT AND WHAT IT IS NOT
1) It is not friendship
2) It is not fellowship
3) It is not befriending
4) It is not a kinship
5) It is professional
6) It is fiduciary - based on trust and benefit for both
7) It is dyadic usually
8) It is built on a clinical foundation
9) No illness No disease No PPR
10) Mostly time limited except in chronic diseases
11) Built on repeated clinical interactions
12) Based on providion of personal care to most of the common health care needs of the client
13) Personal care and continuity care evolve into long term therapeutic relationships